PHVs help millions of people worldwide
Prosthetic heart valves have come a long way since the first successful valve replacement surgery was performed in 1960. Artificial heart valves are surgically implanted to replace damaged or diseased native heart valves that no longer function properly. There are two main types of PHVs in use today - mechanical valves and bioprosthetic (tissue) valves. Each type has advantages and disadvantages that doctors consider when deciding which valve is best for an individual patient.
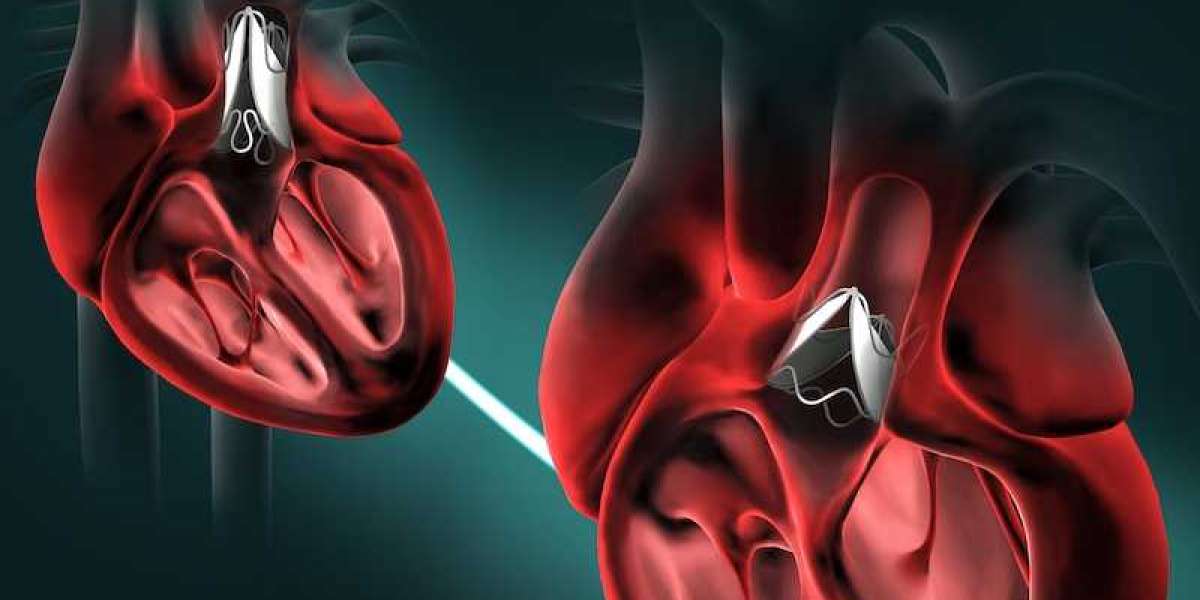
Mechanical heart valves
Mechanical or artificial valves are made entirely from non-biological materials like carbon or metals. The three main types of mechanical valves are caged-ball, tilting disk, and bileaflet valves. Mechanical valves last longer than tissue valves with expected lifespans of 15-20 years. Their rigid, non-biological design also offers very low risks of structural deterioration or infection. However, due to their lack of tissue, mechanical valves require lifelong treatment with blood thinners to prevent blood clots from forming on the valve. This anticoagulation therapy increases the risk of bleeding complications. Mechanical valves also make clicking sounds when opening and closing that some people find bothersome.
Tissue (bioprosthetic) heart valves
Tissue or bioprosthetic valves are constructed from biologically sourced material, usually a pig (porcine) or cow (bovine) tissue treated to reduce negative immune responses. The two most common types are stented porcine valves, where a plastic or metal stent holds up treated pig tissue, and stentless porcine valves, which lack a stent and are molded into the shape of a native human valve. Tissue valves do not require long-term anticoagulation but have more limited lifespans of 10-15 years due to calcification and structural deterioration over time. Younger patients with tissue valves will likely need another replacement surgery within 10-20 years.
Continuous improvements
Technological advancements aim to address the trade-offs between mechanical and tissue valves. Lifestyle-compatible mechanical valves reduce clotting risks with designs like carbon leaflets that limit pannus overgrowth. Bioprosthetic valves now undergo additional fixation treatments and altered material compositions to better resist calcification and degradation. The use of polymeric instead of fixed metal stents further enhances flexibility and durability. Researchers are also developing completely biological engineered valves grown from a patient's stem cells with potential for indefinite lifespans.
Future of transcatheter heart valves
One rapidly developing area is transcatheter heart valve replacement - commonly known as TAVR (transcatheter aortic valve replacement). TAVR allows high-risk surgical patients to receive a new aortic valve through a catheter inserted into blood vessels rather than open-heart surgery. The folded valve is guided by imaging to the defective native valve location then expanded in place. Early clinical outcomes demonstrate TAVR valves work well with less risks than surgery for elderly populations. Advancements now broaden TAVR applications to include mitral, pulmonary, and tricuspid valves beyond just aortic positions. Improved valve designs, delivery catheters, and navigation technologies will continue driving down-risks of TAVR procedures over time.
Personalized prosthetic choices
With many valve options available, doctors consider each patient's particular anatomy, medical history, lifestyle factors, and life expectancy when deciding the best valve type. For example, younger patients are usually given tissue valves to avoid anticoagulation requirements but accept more re-operations risks later in life. Mechanical valves remain preferable for certain patients due to reliability concerns with bioprosthetic durability. New technologies also enable more customized solutions - like the development of hybrid valves that mechanically suspend tissue leaflets or stents adapted for anatomical variations. The future promises even more tailored prosthetic innovations and treatment approaches individualized for optimal patient outcomes.
Monitoring valve performance over time
Regular clinical and imaging follow-ups help monitor prosthetic valve function and structural integrity long-term. Echocardiograms provide data on leaflet mobility, pressure gradients, regurgitation levels and pannus/calcification development. CT and MRI further clarify anatomic relationships. Biological markers also track inflammatory responses. Any deterioration signs prompt additional testing frequency increases while clinical symptoms necessitate careful differential diagnosis between valve, myocardium and conduction system issues. Early detection allows timely valve revision/replacement execution before critical stenosis or regurgitation emerge. Close lifetime surveillance optimizes prosthesis service duration and cardiac reserve preservation.
Prosthetic heart valves have given hope and extended lives for millions over decades. Continuous refinement of materials, designs and surgical methods now provide patients and doctors more options tailored to individual circumstances. Non-invasive technologies continue facilitating minimally invasive therapies. The future promises even less traumatic valve replacements through percutaneous techniques, advanced biomaterials resistant to degradation, tissue-engineered solutions grown from one's own cells and personalized care maximizing each patient's quality of life. Consistent progress maintains momentum toward further minimizing treatment trade-offs thanks to diligent scientific investigation worldwide.
In Summary, prosthetic heart valves play a critical role in restoring normal cardiac function and improving the quality of life for individuals with heart valve disease. These artificial devices are designed to replace damaged or diseased heart valves, restoring proper blood flow and preventing life-threatening complications. With advancements in medical technology, PHVs have become increasingly sophisticated, offering improved durability, functionality, and compatibility with the patient's physiology. Understanding the importance of PHVs underscores their significant contribution to cardiac care and patient well-being.